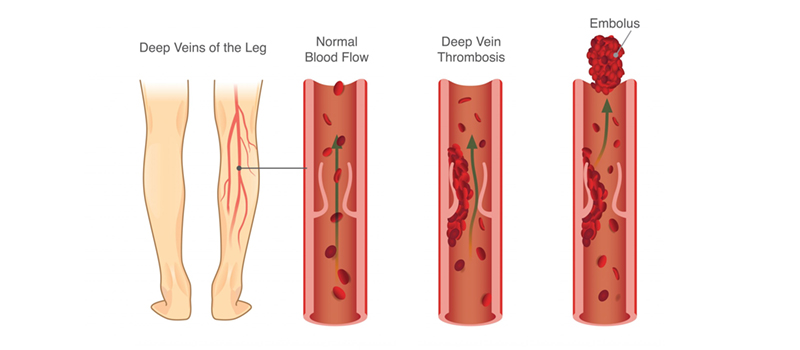
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a blood clot in one of the deep veins in your body. Deep veins are closer to your heart than the superficial veins you can see on the surface of your skin. The two most common places for DVT are in your leg or arm. You may develop it if you sit still for a long time or have severe obesity, high cholesterol, varicose veins, or some other risk factor for DVT.
Symptoms of DVT
- Leg pain
- Swollen leg, especially in the calf and thigh
- Skin discoloration (redness), warmth, or tenderness on the affected area
- Pain when moving your leg, standing up from sitting, or lying down
People with a family history of DVT are at higher risk.
If you have a family history of DVT, you may be at higher risk for developing it. If your parents or siblings have had a blood clot in the past, your chances of getting one are higher than those who don’t have this history.
People with heart disease or those who’ve had an organ transplant are also at higher risk for developing DVT. If you have any of these conditions, talk to your doctor about ways to lower your chances of getting DVT.
If a blood clot breaks loose and travels to another part of your body, it’s called an embolism. An embolism can block blood flow in an artery or vein and cause serious damage if not treated immediately.
Diagnosis
- Ultrasound. An ultrasound can help identify DVT by showing blood clots in the deep veins of your legs.
- MRI. A magnetic resonance imaging (MRI) scan may also be used to diagnose a clot in the deep veins of your legs.
- CT Scan. This type of X-ray uses a computer to create cross-sectional images of the body so that doctors can see its structures more clearly than with other types of scans or X-rays.
- Venogram: This test involves injecting contrast dye into your vein through an intravenous line (IV) while taking images with a special camera called fluoroscopy, which creates an image on film.
Treatment
If you have DVT, your doctor may recommend taking a blood thinner to help prevent new clots from forming and breaking off. This is called anti-coagulation therapy.
Anticoagulants are medications that prevent blood from clotting, which can cause more problems if you have a deep vein thrombosis.
These include:
- Heparin (brand names include Lovenox®)
- Warfarin (Coumadin®)
Surgery
Several surgical options can be considered for patients who don’t respond to or are unable to tolerate anticoagulant therapy.
Thrombectomy involves mechanical removal of the clot, often with a catheter inserted through an artery in your groin or wrist. You’ll need to stay in the hospital for about three weeks afterward and take blood thinners for six months after surgery.
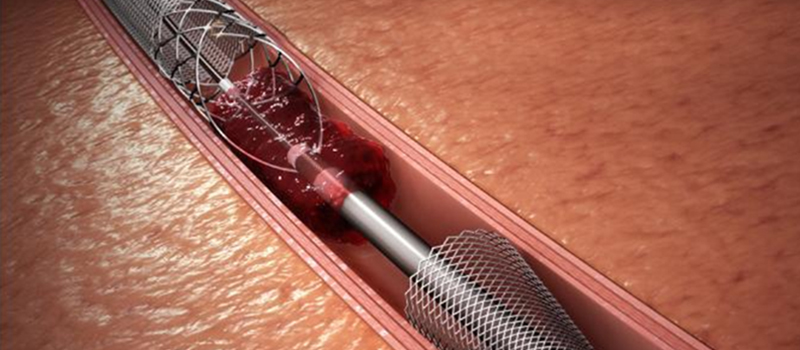
Thrombolysis with a catheter is another option that involves inserting a tube into your blood vessels and injecting special enzymes that break up clots within them.
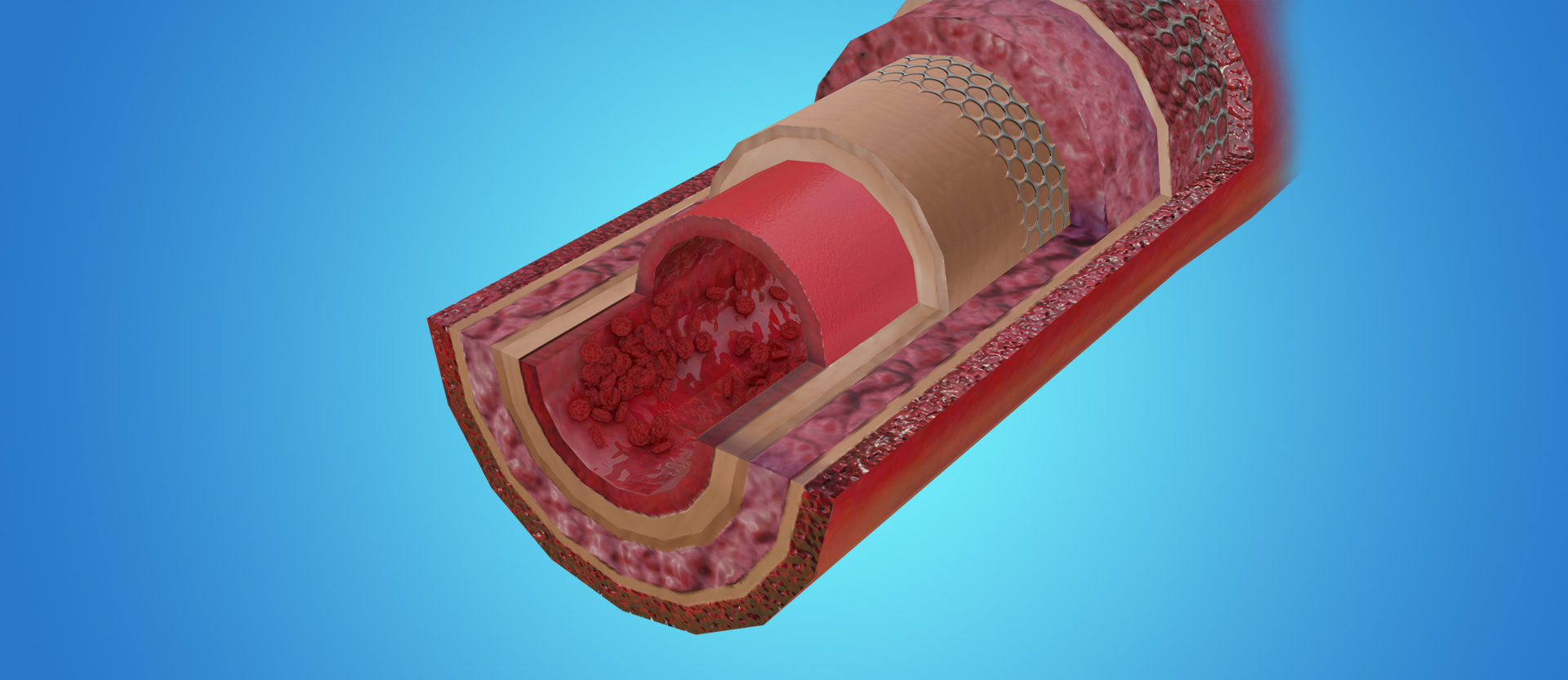
IVC filters are small mesh tubes placed inside your inferior vena cava (the large vein that carries blood from your legs back toward the heart) to help prevent new clots from forming around them and remove any existing ones.
Conclusion
If you or a loved one has experienced Deep Vein Thrombosis, we welcome you to our office. We will work with you to determine the best treatment options. If needed, we can provide education on how to prevent DVT from re-occurring in the future.



